Eyes on the Prize – Why is Eye Care Important?

Dr Duncan Philp is a single CCT ICM trainee in Edinburgh. He is currently doing a Masters in Public Health as his special skills year gaining training in epidemiology.
"Many patients in the ITU are unable to look after their own eyes so it is vitally important that we take care of them on their behalf. They are at higher risk of eye damage both as a result of their acute illness and due to the treatment they receive on ITU.
Sedation and paralysis reduce or stops blinking and can prevent eye closure during sleep, oedema can cause the sclera to swell and protrude from the eye (known as chemosis) and aerosolised respiratory secretions can introduce infection (1, 2). Additionally, prone positioning can cause oedema, corneal abrasions and pressure damage (2, 3).
Over half the intubated patients we look after in ITU suffer some damage to their corneal epithelium (4). This can result in long term problems with sight and have lasting, significant effects on ITU survivors. It is a preventable harm which is well recognised in the literature and yet there is a lack of awareness of it amongst ITU staff (5). It would now be unthinkable to work in an ITU in the UK where there were not bundles and checklists for pressure care, stress ulcer prophylaxis and invasive devises. It is therefore strange that eye care has never attracted the same attention (6).
The Intensive Care Society and the Royal College of Ophthalmology have created an excellent guideline for eye care in the ITU which details risk assessing patients, routine management and management of specific conditions. It can be found here . It is excellent and rather than me repeat everything it says it is probably better to read it yourself!
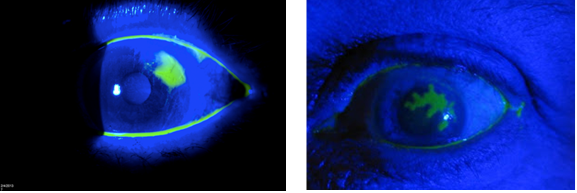
Instead I wanted to talk about some practical tips starting with Fluroscein. Fluroscein and a fundoscope with a blue light is something we should all have on our units and be comfortable using. Fluroscein is taken up into areas of epithelial damage and glows bright green under blue light. It is really important to differentiate between different eye pathologies and is very easy to use. There are some pictures of possible findings below."
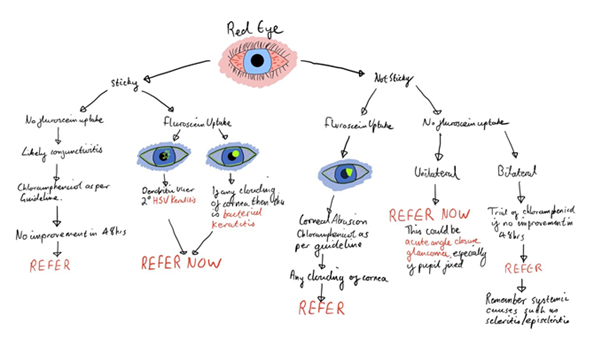
"Next, I wanted to talk about when to refer to an ophthalmologist. Sometimes it is obvious – if there is any pus visible in the eye (hypopyon), any bulging of the eye, any clouding of the cornea, gross chemosis or any suspicion of fungaemia then an immediate referral to ophthalmology is indicated. Sometimes it is less obvious however; red eye is a very common problem with a broad differential. The problem in our patient population is that the assessment and treatment algorithms rely heavily on pain and visual acuity, neither of which are assessable in our patients. Below is my own take on an algorithm for ITU which is from my revision notes and I find useful as a pointer along with the guideline."
Eye damage is a cause of lasting secondary harm which is easy to prevent. There are fantastic guidelines out there and the interventions are simple, all we need to do is think about it. Add it to your ward round checklist (my FLATHUG is now FLATHUGE), add it to the nursing handover and create a link nurse to help spread the word. It would make a great QI project on any ITU.
References
4. Johnson K, Rolls K. Eye Care for Critically Ill Adults. NSW: Agency for Change. 2014.
