Power of the Team in Staff Support

Sara is a Consultant in Emergency Medicine and the Associate Director for Medical Education at the Royal Infirmary of Edinburgh. She has a keen interest in improving staff experience which can take a variety of forms from helping with the set up of Peer Support Networks, promoting Learning from Excellence and Greatix within NHS Lothian and most importantly by regular provision of cake and coffee.
"I love Emergency Medicine, possibly not the most appropriate start to a FICM blog, but it is true. I love the variety, the pace, but most of all I love the people, be they patients or staff, and the teamwork.
I enjoy working with a team who consistently strive to improve patient experience and outcomes. I have been part of many improvement projects, some successful, others not so much. The projects often centre around improving a single variable (usually measured by time) and an assumption that the impact will be improved patient experience. Staff experience is measured as part of the project, but is rarely the focus. Whilst there has been a move toward improving staff experience over the last few years, this has been greatly magnified by the Covid pandemic.
Beside it being good sense there is lots of evidence to show that staff experience impacts patient experience. Workplace stress in healthcare organisations is proven to affect both the quality of patient care and patient satisfaction 1-4. We recognise that work, when good, is a protective factor for your mental health yet contrarily we recognise mental ‘distress’ as a normal reaction for healthcare workers to some of the events we experience5.
Regardless of where you work in healthcare if you ask the question ‘What makes a good day?’ the answers will predominantly focus on colleagues and teamwork. There is enormous power in the support we receive from our colleagues. We all know that our healthcare system is under strain. The result of this is described by Prof Michael West as ‘chronic excessive workload’6 for ourselves and our colleagues. We know that our work can cause us harm. The question is what are we going to do about it?
Our interest in peer support started pre-Covid. There has been some great work done in the US predominantly around providing peer support after adverse events. My colleague Dr Carlyn Davie visited the RISE project in Baltimore and had the privilege of working with its founder Dr Albert Wu. She brought back an enthusiasm for the work that was the driving force behind setting up a pilot peer support project across the Emergency and General Medicine departments of the Royal Infirmary of Edinburgh.
Peer support utilizes the power of our team to support each other through difficult events, work or life related. It gives a structure to the support that many of us already give and receive from colleagues. Importantly it gives the person providing the support a framework to guide the conversation. It gives them permission not to ‘fix’ the problem and instead to listen and guide their colleague to a point where the individual can determine the next steps to be taken.
Our pilot project trained 14 peer supporters from across our Emergency Department and our Acute and General Medicine wards. We also trained members of our board Organisational Development (OD) and Corporate Education teams. The peer supporters came from a variety of disciplines including medical, nursing and administration lines and were trained by our talented Head of Spiritual Care and Bereavement, Duncan MacLaren. The service launched in January 2020, prior to any of us knowing how a pandemic would impact on our home and work lives.
A key part of the framework for our peer support service was to ensure that we had enough support in place for those offering the peer support. Regular supervision sessions have been set up so that peer supporters are given the time and space to reflect on what they have been hearing and the opportunity to problem solve with their colleagues and a trained facilitator. These sessions have proved valuable for the peer supporters both in helping them improve their skills but also in maintaining their own wellbeing. Many of the peer supporters have reflected that they were fulfilling this role previously but without a framework or a support mechanism.
From the start we were aware that measuring the impact of our pilot project would be difficult. Experience from other areas has shown that the number of ‘formal’ peer support contacts is small. The service acts more as a nudge towards a culture of open discussion around the difficulties each of us are experiencing, an acknowledgement that our work can cause us harm and a nod that asking for help when you need it is the right thing to do. The pandemic clearly added another dimension of difficulty to data gathering however we do have good data showing that whilst formal contacts number approximately one a month, the peer supporters feel they are often utilising their skills and that they can identify ‘informal’ support conversations occurring weekly.
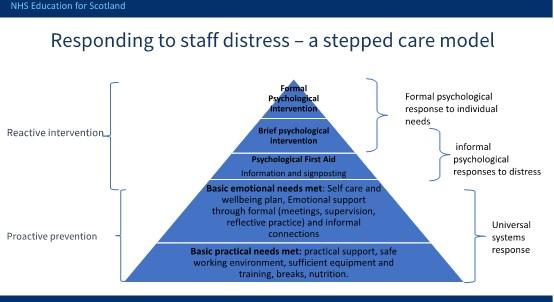
Whilst many projects I have been working on have withered during Covid those based around staff wellbeing and experience have thrived. NHS Education Scotland have developed a framework for responding to staff distress7 which describes the actions we can take to support staff health. It divides these in to those that are ‘proactive prevention’ and those that are ‘reactive intervention’. Peer support really sits on the border between these, it helps us meet the basic emotional needs of our colleagues and it can provide psychological first aid for those who are acutely distressed.
There is interest across our system in being able to provide services that addresses the ‘grey area’ between good mental health and poor mental health requiring formal intervention. Peer support is one aspect of this and the experience of our pilot team, and especially the involvement and support of our OD and corporate education colleagues, has meant that NHS Lothian has adopted the project to scale up and offer across our board and Health and Social Care Partnerships. We are in the process of training 150 peer supporters across our organisations.
The real thrill for me has been in seeing the number of teams and individuals engaging with the project and coming forward for training. On the courses I’ve been facilitating the improvement in skills over the two days has been great to watch and it is a real privilege to hear the experiences and stories from colleagues across our organisations. Their enthusiasm for the concept of a peer support service and their drive to help us make it a reality are infectious. Overcoming the pressures in our system may not be achievable by any one of us individually but supporting our colleagues to have a ‘good day’ is achievable. This will improve both their experience and the experience of the patients we treat.
Our networks and workplaces are full of inspiring colleagues. The set up of local support systems is absolutely within the remit of all teams, even better if your organisation supports a programme of training. Whilst it is unrealistic for us to expect that every day will be a ‘good day’, we need to ensure the good days outweigh the bad and that support is readily available for those who need it. The power of our teams to support each other cannot be underestimated. Positive patient experience comes from positive staff experience, so look after your teams, and importantly look after yourself."
References
- NHS staff management and health service quality [Internet]. GOV.UK. 2011. https://www.gov.uk/government/publications/nhs-staff-management-and-health-service-quality
- NHS Employers. Staff experience and patient outcomes: What do we know? [Internet]. 2014. https://www.nhsemployers.org/-/media/Employers/Publications/Research-report-Staff-experience-and-patient-outcomes.pdf
- The King’s Fund. Employee engagement and NHS performance [Internet]. 2012. https://www.kingsfund.org.uk/sites/default/files/employee-engagement-nh…
- NHS England. Links between NHS staff experience and patient satisfaction: analysis of surveys from 2014 and 2015 [Internet]. 2018. https://www.england.nhs.uk/publication/links-between-nhs-staff-experience-and-patient-satisfaction-analysis-of-surveys-from-2014-and-2015/
- Supporting Clinicians during Covid-19 and Beyond — Learning from Past Failures and Envisioning New Strategies. Jo Shapiro, M.D., and Timothy B. McDonald, M.D., J.D. NEJM DOI: 10.1056/NEJMp2024834
- Caring for doctors, caring for patients. Prof Michael West, Dame Denise Coia. https://www.gmc-uk.org/-/media/documents/caring-for-doctors-caring-for-patients_pdf-80706341.pdf
- NHS Education for Scotland. ‘Responding to staff distress- a stepped care model’ https://learn.nes.nhs.scot/30128/psychosocial-mental-health-and-wellbeing-support/taking-care-of-other-people/responding-to-staff-distress-a-stepped-care-model
