ACCPs
Advanced Critical Care Practitioners are part of the multidisciplinary ICU team
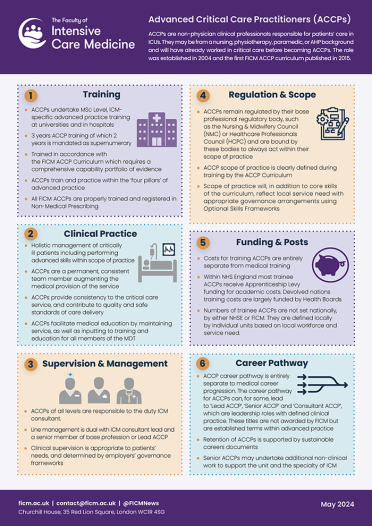
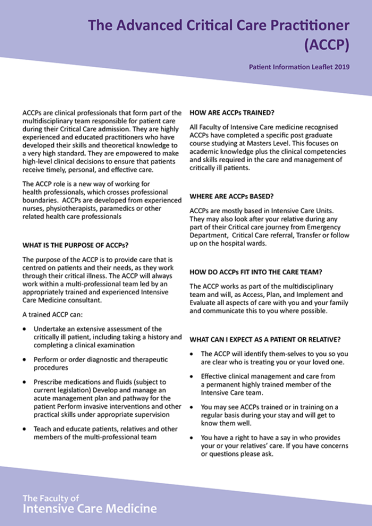
Advanced Critical Care Practitioners (ACCPs) are clinical professionals responsible for patients' care during their critical care admission. They are highly experienced and educated practitioners who have developed their skills and theoretical knowledge to a very high standard. They are empowered to make high-level clinical decisions to ensure that patients receive timely, personal, and effective care.
What are ACCPs?
The ACCP role is a way of working for health professionals, which crosses professional boundaries. ACCPs are currently developed from experienced nurses, physiotherapists, paramedics or other related health care professionals. In the future it is envisaged that ACCPs may also be drawn from other emerging healthcare roles.
ACCPs can
- Undertake comprehensive clinical assessment of a patient’s condition
- Request and perform diagnostic tests
- Initiate and manage a clinical treatment plan
- Provide accurate and effective clinical handovers
- Undertake invasive interventions within the scope of practice
- Provide professional leadership and support within a multi-professional team
- Work autonomously in recognised situations
- Demonstrate comprehensive knowledge across a range of subject areas relevant to the field of critical care
- Critically analyse, evaluate and synthesise different sources of information for the purpose of assessing and managing the care of a critically ill patient
- Apply the principles of diagnosis and clinical reasoning that underlie clinical judgement and decision making
- Apply theory to practice through a clinical decision-making model
- Apply the principles of therapeutics and safe prescribing
- Understand the professional accountability and legal frameworks for advanced practice
- Function at an advanced level of practice as part of the multidisciplinary team as determined by the competency framework
- Apply the principles of evidence-based practice to the management of the critically ill patient
- Understand and perform clinical audit
ACCPs must complete a programme leading to an appropriate Postgraduate Diploma/Masters degree with a Higher Education Institution. Teaching within hospitals is overseen by a Local Clinical Lead (LCL) who holds an honorary appointment with the HEI and is responsible to the HEI for the delivery of the clinical components of training. The Department of Health National Education and Competence Framework for ACCPs can be found in the related downloads section below.
ACCP Information
Core Capabilities Framework
The National Education and Competence Framework for Advanced Critical Care Practitioners was published by the Department of Health in 2008. The framework built on the work of the Changing Workforce Programme development sites that tested the role in clinical practice, the National Practitioner Programme Critical Care Board, the Education and Competence Advisory Party, higher education institutions (HEIs) and clinical colleagues, drawn from a range of backgrounds, with a specific interest in critical care development.
FICM was founded in 2010 and the first edition of the FICM ACCP curriculum published in 2015.
ACCPs, MAPs and the Centre for Advancing Practice
FICM's ACCP Sub-Committee were involved in the early discussions with the Health Education England (HEE) Medical Associate Professionals (MAPs) Oversight Board.
In December 2021, FICM polled the ACCP community (fully trained, registered, and ACCPs in training, as well as the wider community via the National Association of ACCPs) around the future direction for the role. 77% of respondents clearly supported the feeling that active involvement in the MAP agenda had become increasingly less applicable for ACCPs. This tallied with the view of the FICM ACCP Sub-Committee and the MAP Oversight Board.
As such, HEE (now NHSE) and the Faculty agreed in April 2022 that the role of ACCPs would cease to fall under the scope of the MAPs programme and is instead formally aligned with the Centre for Advancing Practice.
ACCPs continue to hold registration with their base profession (e.g. NMC), not the GMC, and are qualified non-medical prescribers.
Want to know more?
Read the ACCP curriculum.